Understanding Semaglutide: Mechanisms and Medical Applications
Semaglutide, a medication that has garnered significant attention in the medical community, represents a pivotal advancement in the treatment of type 2 diabetes and, more recently, obesity. Developed through sophisticated biotechnological methods, this drug mimics the functions of a naturally occurring hormone in the human body, thereby offering a novel approach to managing these chronic conditions.
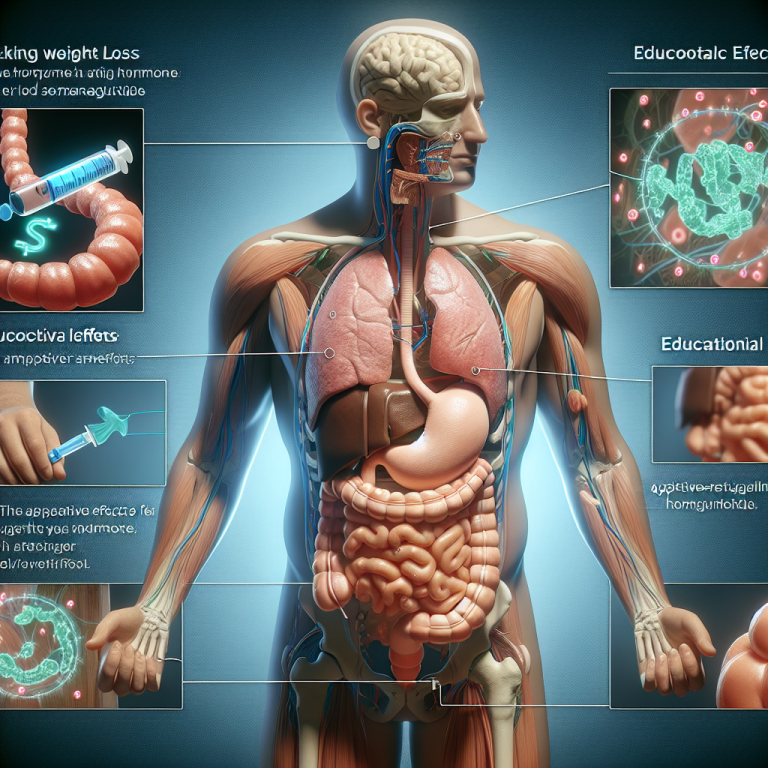
The underlying mechanism of Semaglutide hinges on its structural similarity to glucagon-like peptide-1 (GLP-1), a hormone that plays a crucial role in glucose metabolism. GLP-1 is secreted by the intestines in response to food intake and stimulates the pancreas to release insulin while suppressing glucagon secretion. Insulin and glucagon are hormones that regulate blood sugar levels; insulin decreases blood sugar, while glucagon increases it. By acting like GLP-1, Semaglutide enhances the body's natural insulin release, reduces excessive glucagon production, and slows gastric emptying, which together help in controlling blood glucose levels effectively.
This mechanism provides a substantial therapeutic benefit in managing type 2 diabetes. Patients using Semaglutide can achieve better glycemic control, which is critical in preventing the long-term complications associated with diabetes, such as neuropathy, retinopathy, and cardiovascular diseases. Moreover, unlike many other antidiabetic medications, Semaglutide has a lower risk of causing hypoglycemia, or dangerously low blood sugar levels, because its action is glucose-dependent; it primarily works when there is a rise in blood sugar following meals.
Transitioning from its role in diabetes care, Semaglutide has also emerged as a promising treatment for obesity—a condition linked closely with type 2 diabetes. Obesity results from an energy imbalance and is associated with numerous health risks including hypertension, coronary heart disease, and certain types of cancer. Semaglutide addresses obesity by mimicking the satiety hormone GLP-1, thereby reducing appetite and calorie intake. Clinical trials have demonstrated that when used for weight management, Semaglutide can lead to significant weight loss by decreasing hunger and increasing feelings of fullness after eating. This can be a game-changer for individuals struggling with obesity, especially those for whom diet and exercise alone have not been effective.
The dual benefits of Semaglutide in managing both type 2 diabetes and obesity underscore its potential impact on public health. As these conditions often coexist and exacerbate each other, a single treatment approach that can address both effectively is highly advantageous. It simplifies treatment regimens and can potentially improve patient adherence and outcomes.
However, while the benefits of Semaglutide are clear, it is also important to consider the potential side effects and limitations. Common side effects include gastrointestinal issues such as nausea, vomiting, and diarrhea. These are generally mild to moderate in severity and tend to decrease over time as the body adjusts to the medication. More serious concerns, such as potential risks of thyroid tumors, have been noted in animal studies, though it is not clear if these risks directly translate to humans.
In conclusion, Semaglutide offers a powerful tool in the fight against diabetes and obesity, diseases that impose significant health burdens worldwide. Its ability to regulate blood sugar and reduce weight safely makes it a valuable addition to the therapeutic arsenal. However, careful consideration of its side effects and continuous research into its long-term impacts are essential to fully harness its potential while ensuring patient safety. As with any medical treatment, a balanced approach that considers both the benefits and risks is crucial for optimal health outcomes.
Semaglutide in Weight Management: Efficacy and Patient Experiences

Semaglutide, a medication initially approved for the treatment of type 2 diabetes, has recently garnered significant attention for its efficacy in weight management. This drug, administered via injection, mimics a hormone that targets areas of the brain involved in regulating appetite and food intake. As obesity continues to be a major health challenge globally, the potential of semaglutide to aid in substantial and sustained weight loss is a promising development for both clinicians and patients.
Clinical trials have demonstrated that semaglutide significantly reduces body weight by decreasing appetite and caloric intake. In a landmark study, participants receiving semaglutide lost approximately 15% of their body weight on average, a result that far surpasses the outcomes seen with other pharmacological agents. This level of efficacy positions semaglutide as a leading option in the pharmacotherapy of obesity, a critical component in the multi-disciplinary approach to tackling this complex and chronic disease.
Patients treated with semaglutide have reported not only significant weight loss but also improvements in quality of life and a reduction in risk factors for several chronic diseases. These include hypertension, type 2 diabetes, and cardiovascular disease, which are often associated with obesity. Moreover, the weight loss achieved with semaglutide has been shown to be sustainable over longer periods, provided that patients adhere to their treatment regimen. This aspect is particularly important, as maintaining weight loss is often more challenging than losing the weight initially.
However, the experience of patients on semaglutide varies, and the medication is not devoid of side effects. Common adverse reactions can include gastrointestinal issues such as nausea, vomiting, diarrhea, and constipation. These side effects are generally transient and tend to diminish over time as the body adjusts to the medication. It's crucial for potential users to have realistic expectations and to discuss these side effects with healthcare providers to manage them effectively.
The decision to use semaglutide for weight management should also consider individual factors such as the patient's overall health status, their risk profile for obesity-related complications, and their previous attempts at weight loss. Healthcare providers typically recommend a comprehensive approach that includes lifestyle changes such as diet modification, increased physical activity, and behavioral interventions in conjunction with semaglutide treatment. This holistic approach ensures that weight loss is both achieved and maintained, enhancing overall health outcomes.
Furthermore, as more people use semaglutide, real-world data continues to accumulate, providing deeper insights into its long-term impacts and effectiveness across diverse populations. This information will be crucial for tailoring treatments to individual needs and optimizing weight management strategies.
In conclusion, semaglutide represents a significant advancement in the treatment of obesity. Its ability to induce weight loss effectively and sustainably can be a game-changer for many patients struggling with obesity. However, it is not a magic bullet. Successful weight management with semaglutide requires careful consideration of potential side effects, realistic expectations from patients, and a commitment to comprehensive lifestyle changes. As the medical community gathers more evidence and refines treatment protocols, semaglutide stands to play a pivotal role in the ongoing battle against obesity, promising not just weight loss but also enhanced overall health and well-being.
The Future of Semaglutide: Emerging Research and Potential Therapies
Semaglutide, a drug initially approved for the treatment of type 2 diabetes, has recently gained significant attention due to its potential in other therapeutic areas. As research progresses, the future of semaglutide looks promising, with studies exploring its application in obesity management, cardiovascular health, and even neurological disorders.
The journey of semaglutide began with its ability to regulate blood sugar levels in diabetic patients. However, its mechanism of action, primarily through mimicking an incretin hormone that stimulates insulin secretion, has broader implications. For instance, semaglutide has shown remarkable efficacy in weight loss among individuals with obesity. Clinical trials have consistently demonstrated that semaglutide, administered weekly via injection, can lead to substantial weight reduction in obese and overweight patients. This effect is not only beneficial for weight management but also aids in mitigating the risks associated with obesity, such as hypertension and dyslipidemia.
Transitioning from metabolic health to cardiovascular wellness, semaglutide has opened new avenues in cardiology. Research has indicated that it can improve cardiovascular outcomes, reducing the risk of heart attack, stroke, and cardiovascular death in diabetes patients with established heart disease. This potential makes semaglutide a dual-purpose therapeutic agent in the realm of metabolic and heart diseases, offering a holistic approach to treating patients with multiple comorbidities.
Moreover, the scope of semaglutide is expanding into the domain of neurology. Preliminary studies suggest that semaglutide may exert protective effects on brain health. Researchers are investigating its capacity to influence pathways involved in neurodegenerative diseases such as Alzheimer's and Parkinson's. Although these studies are in their nascent stages, they represent a significant leap towards understanding how metabolic treatments can intersect with neurological pathways.
Emerging research also points to the role of semaglutide in addressing Non-Alcoholic Steatohepatitis (NASH), a liver condition that leads to cirrhosis in severe cases. Semaglutide's ability to improve insulin sensitivity and reduce inflammation could potentially slow the progression of NASH, thereby preventing the development of more severe liver diseases. This is particularly crucial considering the limited treatment options currently available for NASH, making semaglutide a potential game-changer in hepatology.
As we look towards the future, the versatility of semaglutide may also lead to its incorporation into personalized medicine. Given its varied applications, treatment protocols could be tailored based on individual patient profiles, enhancing efficacy and minimizing side effects. This approach would not only improve patient outcomes but also reduce healthcare costs by targeting therapy more precisely.
In conclusion, semaglutide is on a trajectory to become more than just a treatment for diabetes. Its expanding role in medical science speaks to a broader trend of repurposing medications to serve multiple health needs. As ongoing and future studies continue to uncover its full potential, semaglutide could well be at the forefront of a new era in medical therapy, transforming lives across multiple spectrums of disease. The implications of such a development are profound, indicating a significant shift in how we approach disease management and patient care in the years to come.