Semaglutide And Weight Loss: Exploring Its Efficacy And Mechanisms
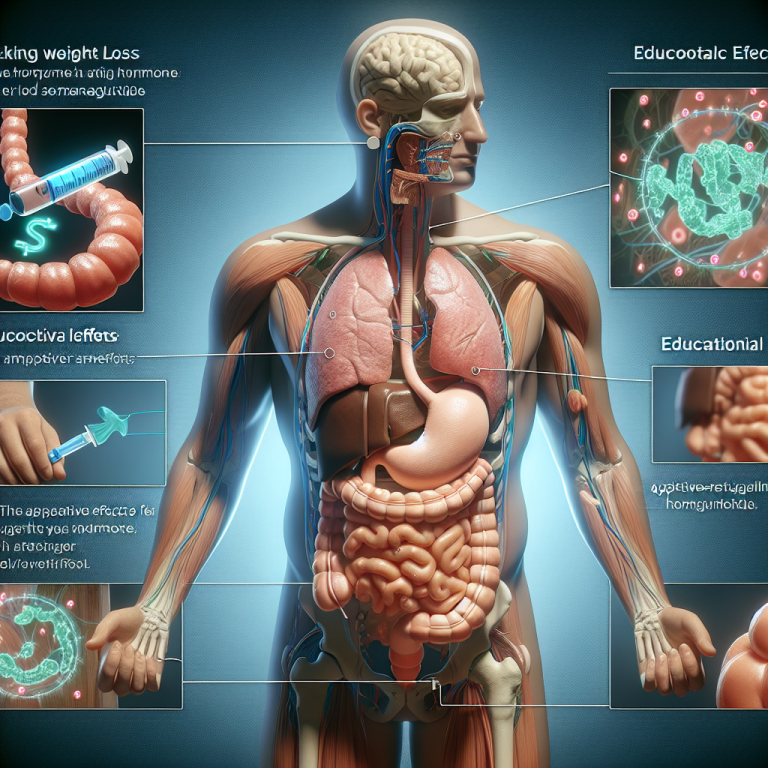
Semaglutide, a medication initially approved for the treatment of type 2 diabetes, has recently gained significant attention for its potential benefits in weight management. The drug, which mimics a hormone called glucagon-like peptide-1 (GLP-1), plays a crucial role in regulating insulin secretion and appetite. This dual action not only helps in controlling blood sugar levels but also in reducing body weight, making it a promising option for individuals struggling with obesity.
The efficacy of semaglutide in weight loss has been demonstrated through several rigorous clinical trials. In these studies, subjects receiving semaglutide experienced a notable reduction in body weight compared to those who were given a placebo. The weight loss effects of semaglutide are primarily attributed to its ability to decrease appetite and caloric intake. By mimicking GLP-1, semaglutide increases the production of insulin, which helps lower blood sugar levels, and decreases glucagon secretion, which in turn reduces hunger.
Moreover, semaglutide influences the brain's appetite-regulating pathways. It acts on areas of the brain that control appetite and food intake, leading to a reduced desire to eat. This neurological impact is significant as it addresses one of the fundamental challenges in weight management: the management of hunger and satiety. The ability of semaglutide to help individuals feel fuller sooner and stay satisfied for longer after meals can lead to a substantial decrease in overall calorie consumption.
Another aspect of semaglutide's action is its impact on gastric emptying—the rate at which food leaves the stomach and enters the small intestine. By slowing this process, semaglutide can prolong the feeling of fullness after eating. This delayed gastric emptying contributes further to a decrease in food intake and, consequently, weight loss.
Clinical outcomes have shown that the weight loss achieved with semaglutide is not only significant but also sustainable over time. In one of the pivotal trials, participants continued to lose weight progressively over the course of treatment, which lasted up to 68 weeks. This sustained weight loss is crucial for the long-term management of obesity, a chronic condition that requires ongoing treatment strategies.
However, while the benefits of semaglutide in promoting weight loss are clear, it is important to consider potential side effects. Common adverse effects include gastrointestinal issues such as nausea, diarrhea, and constipation. These side effects are generally mild to moderate and tend to decrease over time as the body adjusts to the medication. Nevertheless, it is essential for individuals considering this treatment to discuss these potential side effects with their healthcare provider.
In conclusion, semaglutide represents a significant advancement in the treatment of obesity. Its ability to modify appetite and food intake through multiple mechanisms—not only improving glycemic control but also promoting weight loss—makes it a valuable tool in managing this complex and challenging condition. As obesity continues to be a major health concern worldwide, medications like semaglutide that can effectively address both the physiological and behavioral aspects of this disease are of great importance. With ongoing research and clinical use, semaglutide continues to show promise, potentially changing the landscape of obesity treatment for many individuals.
Semaglutide As A Treatment For Type 2 Diabetes: Benefits And Considerations

Semaglutide, a relatively new medication approved for the treatment of type 2 diabetes, has garnered significant attention for its efficacy and dual benefits. This injectable medication, derived from the human glucagon-like peptide-1 (GLP-1), not only enhances the body’s ability to produce insulin but also suppresses appetite, which can be particularly beneficial for patients struggling with weight management—a common challenge among those with type 2 diabetes.
The primary mechanism through which semaglutide operates involves boosting the pancreas' production of insulin when blood glucose levels are high. Insulin is crucial for regulating blood sugar levels, and its increased availability helps to mitigate the spikes in blood glucose that typically occur after meals. Additionally, semaglutide slows gastric emptying, which contributes to decreased appetite and, over time, leads to weight loss. This aspect of semaglutide's action is especially pivotal, considering the close link between obesity and the development of type 2 diabetes.
Clinical trials have consistently shown that semaglutide significantly reduces hemoglobin A1c—a marker for long-term glucose control—by up to 1.5% when used as a standalone treatment. When combined with other diabetes medications, such as metformin, the effects can be even more pronounced, making it a versatile addition to diabetes management strategies. Moreover, the weight loss experienced by patients on semaglutide is not only a direct result of reduced appetite but also from the improved metabolic effects facilitated by better insulin control.
However, while the benefits of semaglutide are clear, there are several considerations that must be taken into account. Firstly, the medication is administered through weekly injections, which might be a deterrent for those who are uncomfortable with needles. Secondly, there are potential side effects associated with its use. Common adverse reactions include gastrointestinal issues such as nausea, vomiting, diarrhea, and constipation. These side effects are generally transient and tend to diminish over time as the body adjusts to the medication.
Further, there are more serious but rare risks linked to semaglutide, including thyroid tumors. Studies in rodents have shown a higher incidence of thyroid C-cell tumors; however, it is unclear whether this risk is directly translatable to humans. As a precaution, semaglutide is not recommended for individuals with a personal or family history of medullary thyroid carcinoma or those who have Multiple Endocrine Neoplasia syndrome type 2.
Patients considering semaglutide as a treatment option should also be aware of its cost. As a newer medication, it can be more expensive than older diabetes drugs, and insurance coverage may vary, which could make it less accessible for some individuals.
In conclusion, semaglutide represents a significant advancement in the treatment of type 2 diabetes, offering substantial benefits in terms of both glucose control and weight loss. Its ability to improve several markers of diabetes severity and its potential to impact long-term health outcomes positively make it a compelling option for many patients. However, the decision to use semaglutide should involve a thorough discussion with a healthcare provider, considering the potential side effects, costs, and individual patient needs and circumstances. Such a balanced approach will ensure that each patient receives the most appropriate and effective treatment for their specific situation.
The Future Of Semaglutide: Potential Uses Beyond Diabetes And Obesity
Semaglutide, originally developed for the treatment of type 2 diabetes, has recently garnered significant attention for its potential in addressing other serious health conditions, including obesity. This glucagon-like peptide-1 (GLP-1) agonist, by mimicking an intestinal hormone that helps regulate blood sugar, has not only proven effective in controlling glycemic levels but also in promoting weight loss. The versatility of semaglutide opens up a plethora of possibilities for its application in medicine, particularly in areas where current treatments are limited or non-existent.
The exploration of semaglutide in the field of obesity has shown particularly promising results. Clinical trials have demonstrated that it can lead to substantial weight loss by reducing appetite and food intake. This effect is achieved through its action on the brain's appetite-regulating pathways, making it a groundbreaking tool in the fight against obesity, which is often resistant to both lifestyle changes and medication. However, the potential applications of semaglutide extend beyond these already significant uses, venturing into other medical conditions that are linked to high body weight and metabolic dysfunction.
One of the potential future uses of semaglutide could be in the management of non-alcoholic fatty liver disease (NAFLD), a condition closely associated with obesity and diabetes. NAFLD, characterized by the accumulation of fat in liver cells in individuals who drink little or no alcohol, is a growing global health concern due to its potential to lead to more severe liver diseases such as cirrhosis and liver cancer. Early research suggests that the weight loss induced by semaglutide could play a crucial role in reducing liver fat, thus improving or even reversing the condition. This hypothesis is currently under rigorous investigation, with several studies aiming to confirm the efficacy and safety of semaglutide for patients suffering from NAFLD.
Moreover, semaglutide's impact on cardiovascular health is another area under intense scrutiny. Patients with type 2 diabetes and obesity are at a heightened risk of developing cardiovascular diseases. Semaglutide has shown promise in not only mitigating these risks through effective management of blood glucose levels and body weight but also potentially improving overall heart health. Ongoing studies are focused on understanding how semaglutide can influence factors like cholesterol levels, blood pressure, and arterial health, all of which are critical components of cardiovascular wellness.
Beyond these applications, researchers are also intrigued by the possibility that semaglutide could be beneficial in the treatment of neurodegenerative diseases such as Alzheimer’s disease. The theoretical framework supporting this hypothesis lies in the drug's potential to improve insulin resistance and reduce inflammatory markers, both of which have been implicated in the pathogenesis of Alzheimer’s disease. Although still in the preliminary stages, this research avenue could redefine the treatment landscape for neurodegenerative conditions, offering hope where there is currently limited progress.
In conclusion, semaglutide stands out not only as a revolutionary treatment for diabetes and obesity but also as a beacon of hope for various other debilitating conditions. Its evolving role in medicine could potentially lead to breakthroughs in areas where traditional treatments have failed, offering improved health outcomes and quality of life for patients across multiple disease spectrums. As research continues to unfold, the full scope of semaglutide’s impact on health care remains a promising field of discovery.